Abstract

Background: End stage renal disease (ESRD) is a common complication of sickle cell disease (SCD), contributing to 14% mortality. Most patients with ESRD are managed with dialysis. The relative risk of mortality in hemodialysis (HD) versus peritoneal dialysis (PD) may be influenced by the primary cause of ESRD (Vonesh et al, 2004). The purpose of this study is to compare patients with ESRD primarily caused by SCD (SCD-ESRD) to non-SCD-ESRD controls and to evaluate the association of dialysis type with mortality and hospitalization in SCD-ESRD patients.
Methods: This was a retrospective study of SCD-ESRD patients newly initiated on dialysis in the United States Renal Data System between January 1, 2006 and December 31, 2013. SCD-ESRD patients were identified by ICD-9 codes. A sample of 5% of African Americans with incident ESRD caused by conditions other than SCD (non-SCD-ESRD cohort) initiated within the same timeframe were randomly selected as controls. Patient demographics, comorbidities, and dialysis type were compared between SCD and controls. Patient demographics, clinical characteristics, and outcomes were compared between HD and PD patients in the SCD-ESRD cohort. Chi-square, t-test, and Wilcoxon rank sum tests were used for comparative analysis. Survival times were estimated by Kaplan Meier curve and compared using log rank test.
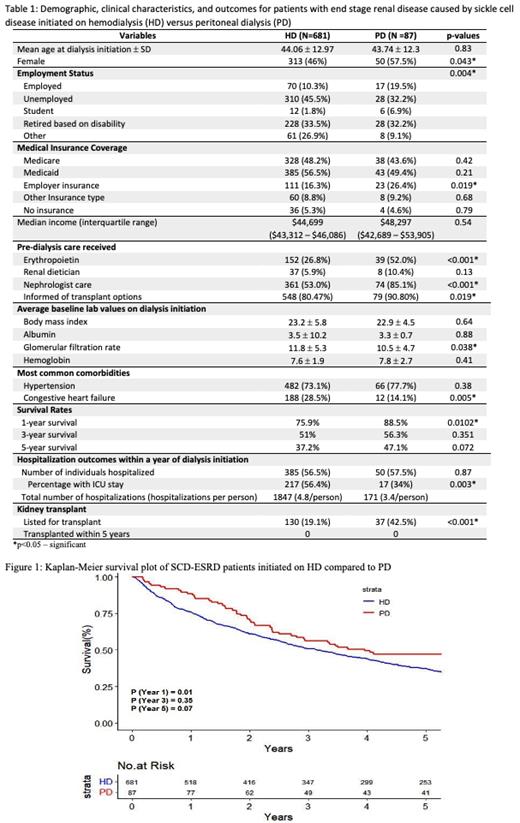
Results: 768 SCD-ESRD and 12,402 non-SCD-ESRD patients were included in analysis. SCD-ESRD patients started dialysis at a younger age (44±12.9 vs 58.6±15.4 years; p<0.001), were more likely to be unemployed (44% vs 29.7%; p<0.001) and have Medicaid insurance (55% vs 33%; p<0.001). Most common comorbidities in SCD-ESRD patients were hypertension (71%) and congestive heart failure (26%) and in controls were hypertension (89.3%) and diabetes (61.3%). SCD-ESRD patients had twice the odds of being initiated on PD compared to controls (11.3% vs 5.7%, OR 2.11, p<0.001). Demographics, comorbidities, laboratory values, access to nephrology care prior to dialysis initiation, survival, hospitalization, and kidney transplantation of HD and PD patients in the SCD-ESRD cohort are shown in Table 1. Kaplan Meier survival plot is shown in Figure 1. PD patients were more likely to be female, have full time employment and employer insurance, be students, have lower glomerular filtration rate, and have congestive heart failure as a comorbidity. They were also 1.6 and 1.9 times more likely to have been seen by a nephrologist and received erythropoietin prior to dialysis initiation respectively (p<0.001). PD patients had significantly better survival rates at year 1 (88.5% vs 75.9%, p=0.01). Survival rates were still higher in PD patients at years 3 and 5 although not statistically significant. HD and PD patients were hospitalized equally within a year of dialysis initiation however, HD patients had more intensive care unit (ICU) stays (p=0.003) and ~1.5 times the number of hospitalizations per person. More PD patients had been informed about (90.8% vs 80.47%, p=0.019) and listed for (42.5% vs 19.1%, p<0.001) transplant although no patients in this study had undergone a kidney transplant within the 5 year follow up.
Discussion: SCD-ESRD patients in this study were more likely to be started on PD compared to non-SCD-ESRD patients. This could be explained by the younger age of SCD-ESRD patients as younger individuals are more likely to be started on PD in the general ESRD literature. SCD-ESRD patients started on PD had better survival and hospitalization outcomes particularly within the first year of dialysis initiation when mortality and morbidity is known to be high in ESRD. These results suggest a survival benefit of PD over HD in SCD-ESRD patients. This could perhaps be explained by decreased likelihood of vaso-occlusive events due to less fluid shifts and thus hematocrit fluctuations in the PD group (Boyle et al, 2016). A limitation of our study is that we do not have data on the possibility of individuals switching dialysis modalities (crossovers) over the course of follow up that could bias survival rates in either direction. A next step would be to look at the same outcomes in individuals who switch. Moreover, a prospective observational study or randomized control trial could further evaluate differential survival rates in HD versus PD initiation in SCD and inform guidelines in SCD-ESRD care.
Acknowledgement: Support was provided to MKS by the Minority Resident Hematology Award Program.
Achebe: Pharmacosmos: Membership on an entity's Board of Directors or advisory committees; Fulcrum Therapeutics: Consultancy; Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract